Leucorrhoea (White discharge)
What is Leucorrhoea?
Leucorrhoea, also known as the white vaginal discharge is a very common condition that has been experienced by women of all ages, at some time or the other.
The amount of discharge may increase due to vaginal infection, and it may disappear and reappear from time to time. This discharge can keep occurring for years, in which case it becomes more yellow and foul-smelling. It is usually a non-pathological symptom secondary to inflammatory conditions of the vagina or cervix.
Symptoms & Causes
Symptoms
Main symptoms of the disease are excessive vaginal discharge, pain in the thighs and calf muscles and burning micturition etc. The vaginal discharge colour may be whitish, yellowish, reddish and blackish.
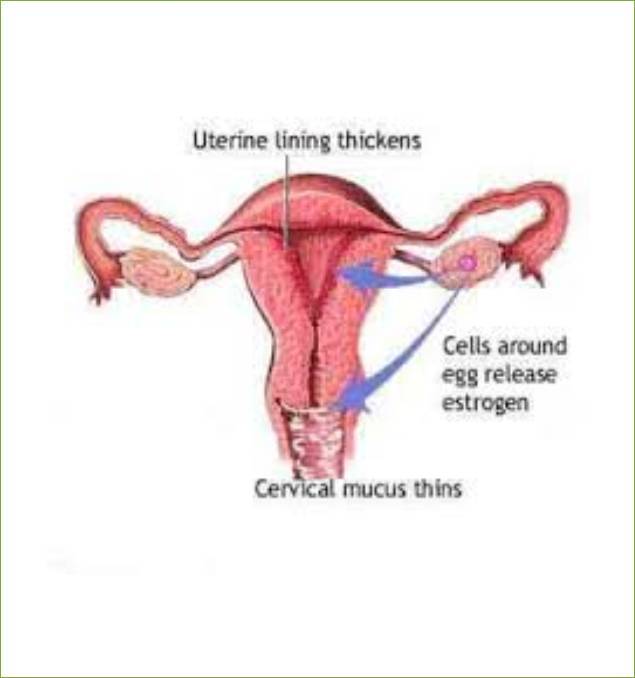
The vagina normally contains bacteria. Bacterial growth is controlled and affected by many different factors, such as acid level (pH) and hormones. Anything that upsets this balance may increase your risk of infection or overgrowth of any of the normal bacteria or by yeast.
Causes
The vagina normally contains bacteria. Bacterial growth is controlled and affected by many different factors, such as acid level (pH) and hormones. Anything that upsets this balance may increase your risk of infection or overgrowth of any of the normal bacteria or by yeast.
Possible triggers include:
- Poor Hygiene
- Anaemia
- Antibiotic use
- Birth control pills
- Douching
- Diabetes
- Pregnancy
- Stress
- Tight or synthetic undergarments
Vaginal Discharge
About Vaginal discharge:
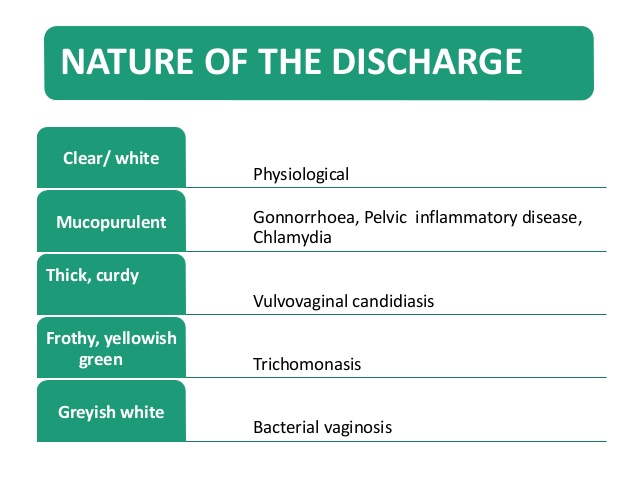
Sexually transmitted diseases such as gonorrhea or Chlamydia also can cause vaginal discharge. Other possible noninfectious causes include inflammation or irritation of the vagina from a scented product such as soap, douches, pads or tampons; diabetes; or low estrogen levels as in menopause (atrophic vaginitis).
Vaginal discharge may result from infection with:
Yeast, also called Candida, a type of fungi that is part of the normal flora of human skin but can also cause infections. Gardnerella, a type of bacteria found normally in the female genital tract that is the cause of bacterial vaginosis. Trichomonas, a type of protozoa, an organism made up of one cell.
Treatment
Infections are treated with antibiotics. Often just one dose of antibiotics by mouth is enough. Another option is to use antibiotics in vaginal cream or gel form, especially if you have significant side effects when you take antibiotics by mouth. Also, the vaginal cream can be more soothing for the inflamed, sore vaginal lining.
If you are diagnosed with bacterial vaginosis or trichomoniasis, your doctor may prescribe an antibiotic called metronidazole (Flagyl). If your doctor suspects you have a sexually transmitted disease based on your history and physical exam, you may be given antibiotics by injection and by mouth in the office before the tests results can confirm the diagnosis.
If you have recurrent yeast infections and recognize the symptoms, you may use over-the-counter antifungal creams without a prescription. If your symptoms do not improve, see your doctor for an exam to confirm the diagnosis and change the treatment.
Atrophic vaginitis may develop with hormonal changes, for example, during breastfeeding after pregnancy or while using certain types of hormonal contraceptives. More commonly, it occurs during or after menopause.
After menopause, estrogen therapy may be taken by mouth or vaginally. Vaginal administration exposes you to lower levels of hormones. For mild cases, using a water-based lubricant may be enough. If you use hormonal contraception, changing the type contraception may help improve symptoms.
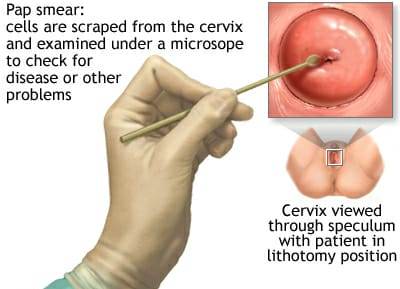
You will then have a pelvic exam. Your doctor will use a device called a speculum to look at the cervix directly. During the pelvic exam, a sample of the discharge is collected for testing. By looking at the discharge under a microscope in the office, your doctor can diagnose yeast infection, bacterial vaginosis or trichomonas infection right away and start treatment. Based on the appearance of the vaginal walls, your doctor may make a diagnosis of atrophic vaginitis.
Your doctor will check the tenderness of your cervix, uterus or ovaries by placing his or her fingers inside your vagina. Tenderness may indicate that you have a sexually transmitted disease or pelvic inflammatory disease. Diagnosing gonorrhea or Chlamydia requires the results of laboratory tests, which may take a few days.
With good perineal hygiene, plenty of fluids and identification of the cause and appropriate treatment on can prevent Leucorrhoea and recurrence.
OPD Timings
Dr. Mandar R Gadgil
| Mon – Fri | - | 4:30 PM - 7:30 PM w.e.f. 27th August 2022 |
| Saturday | - | 10:00 AM - 11:30 AM |
OPD Timings
Dr. Maithilee Gadgil
| MON – SAT | - | 10:00 AM - 12:30 PM |
| MON – FRI | - | 4:30 PM - 07:00 PM w.e.f. 27th August 2022 |
Any Question Or Query
Feel free to ask for your any Question or Query /
Book An Appointment
Appointment
To book appointment call us on